Lupine Publishers Pediatrics and Neonatology
Abstract
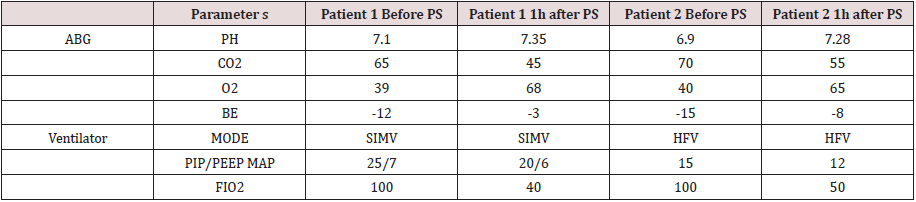
Pulmonary hemorrhage (PH) is a life threatening condition in newborns, especially preterm infants. Surfactant replacement might be helpful to improve lung function and reduce the ventilation support in infants with PH. We report two premature infants (one with early onset PH and one with late onset PH) who have been successfully rescued by administering surfactant (Calsurf) after an acute episode of bleeding. Both of the 2 infants survived, and surfactant administration showed improvement in mean airway pressure and oxygenation indices. In the current study Calsurf was found effective in the treatment of both early PH and late PH in premature infants. There were no potential side effects were found in our study.
Keywords: Premature infants; Pulmonary hemorrhage; Surfactant
Introduction
Pulmonary hemorrhage (PH) is a life threatening condition occurring to 1-12/1000 live births, with rates increasing to 50/1000 live births in risk groups, such as prematurity, intrauterinegrowth restriction (IUGR), patent ductus arterosus (PDA) and/or sepsis [1]. Small gestational age, low birth weight, low agar score at 1 and 5 min, severe respiratory distress syndrome (grade 3 or 4) and use of surfactant replacement are risk factors of PH [2]. Currently the treatment of PH includes stopping pulmonary hemorrhage by epinephrine spraying through an ET, treating secondary RDS by optimal ventilation settings with or without surfactant [3]. On one hand, pulmonary hemorrhage is thought to be a complication of surfactant therapy because surfactant can rapidly lower the intrapulmonary pressure, which facilitates left to right shunting through PDA and an increase in pulmonary blood flow. Thus, clinicians might hesitate to administer surfactant again in neonates with PH. While on the other hand, the presence of hemoglobin, red cell membrane lipid and serum proteins can increase surface tension resulting from surfactant dysfunction and cause secondary RDS [4]. Surfactant replacement might be helpful to improve lung function and reduce the ventilation support. Calsurf has been used in China for several years [5]. Calsurf is a newborn bovine lung surfactant extract as a lyophilized powder in a 70mg/vial. The clinical trials in China by Kong et al. found that the prophylactic use of a domestic surfactant preparation is better than early surfactant treatment in improving the pulmonary status and decreasing the incidence of severe RDS and duration of mechanical ventilation [6].
Case Report
Case1: Early onset of PH
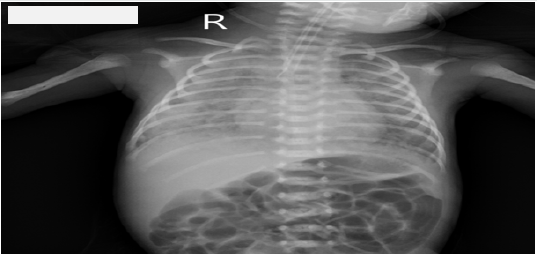
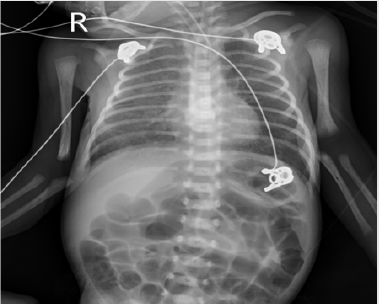
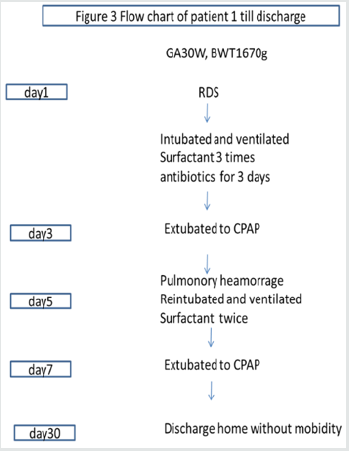
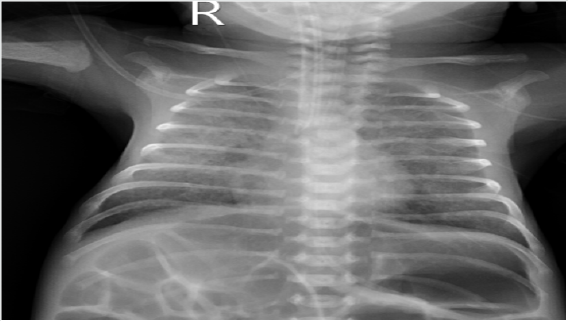
A 30-week male neonate with birth weight of 1670 grams was admitted in neonatal intensive care unit. He showed respiratory distress shortly after birth and was diagnosed of grade 4 respiratory distress syndrome (RDS) by chest X ray. Three doses of surfactant (Calsurf, Shuanghe Famaceutics, China, 80mg/kg.d)were given and he was successfully extubated to SiPAP on day 3. On day 5 of age, the neonate developed profuse PH. He showed desaturation (SpO260%) and when intubated, a large amount of fresh blood was noticed in the endotracheal tube. Chest X ray showed PH (Figure 1). Coagulation tests were normal. Echo showed no PDA. The neonate was put on conventional ventilator with high setting (SIMV, 25/7, FiO21.0) and SpO2 fluctuating from 80-90% (Oxygen indice was 40, see Table 1). Two doses of Calsurf (40mg/kg with dosing interval of 12hr) were given. Clinical and radiological improvement (Figure 2) were found after 24hr of surfactant treatment (Oxygen indice was 170). The neonate was successfully extubated on day 7. At the meanwhile, antibiotics, total fluid limitation were also given to this patient. This infant discharged home on day 30 (CGA 34W) without BPD, PVL and ROP. Flow diagram of the patient till discharge was shown on (Figure 3).
Case 2: Late onset of PH
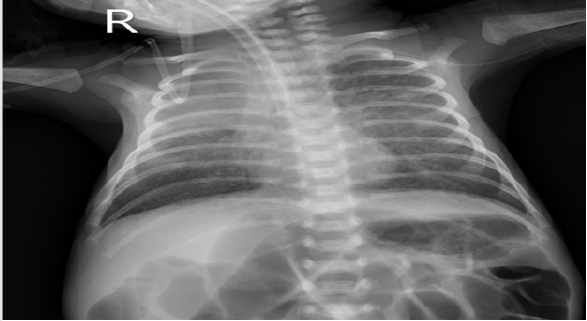
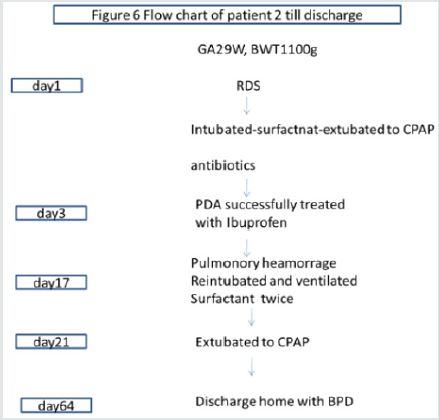
A 29-week neonate born to a mother with nephritic syndrome was admitted in neonatal intensive care unit. His birth weight was 1100 grams. He showed respiratory distress shortly after birth and diagnosed of grade 2 RDS. INSURE (Intubate-surfactantextubate to SiPAP) technique was used. Patent ductus arteriosus, hyperbilirubinemia, Apnea and sepsis complicated with initial course. On day 17th of life, the neonate developed PH and desaturation (SpO250-60%). He was intubated immediately, and a large amount of fresh blood was noticed in the endotracheal tube. Chest X ray showed PH (Figure 3). The ventilator settings on him were HFV, MAP15, FiO21.0 to get the saturation around 90% (Table 1). Lab results showed that this neonate had severe infection. Two doses of Cal surf (60mg/kg with dosing interval of 12hr) were given. Besides ventilation and PS, antibiotics and RBC blood transfusion were also given to this neonate.
Clinical and radiological improvement (Figure 4) were found after 24hr of surfactant treatment. The neonate was successfully extubated on day 21. This infant discharged home on day 64 (CGA 38W) with moderate BPD, but without PVL and ROP
Discussion
Pulmonary hemorrhage is a life-threatening condition and more prevalent in premature newborns, and is associated with mechanical ventilation, PDA, infection and previous use of blood components [2]. Both of our two cases are premature newborns, one suffered from PH shortly after birth (5th day of life), the other one suffered from PH on day 17th of life, most probably due to severe nosocomial infection (Figure 5 & 6). Different approaches have been proposed for the management of PH, including stopping pulmonary hemorrhage by epinephrine spraying through an ET, treating secondary RDS by optimal ventilation settings with or without surfactant [3]. Invitro study showed that the presence of surfactant impaired coagulation by decreasing platelet aggregation and increasing prothrombin time (PT). Whole blood thromboelastogram studies also showed a trend towards lengthening of clotting time with increased surfactant concentration and lower clot strength [5]. Thus, clinicians might hesitate to administer surfactant again in neonates with PH. PH has been effectively managed by using surfactant instillation. Senol et al. reported two kinds of natural surfactants improved oxygenation when administered for PH in very low birth weight infants [6]. In majority of cases studies surfactant was given as a treatment of PH in the first few days of life (early onset of PH) [6,7]. However, in the present study both early onset of PH and late onset of PH were successfully rescued by surfactant therapy. In our two cases, Calsurf was used in both cases and Calsurf administration showed improvement in mean airway pressure and oxygenation indices. Calsurf is a natural surfactant produced by Shuang he Famaceutics, China. Its active ingredient is the phospholipid fraction obtained from bovine lung. Of the surfactant lipid, total phospholipid is more than 80%, of which phosphatidylcholine is no less than 55%. Calsurf has been found effective in the treatment of respiratory distress syndrome among premature infants in Chinese population [8,9]. In the current study Calsurf was found effective in the treatment of PH in premature infants.
Conclusion
Surfactant (Calsurf) therapy was found to be safe and effective in both early PH and late PH in preterm infants. Further randomized controlled trail would be useful for identification of potential benefit.
For more Lupine Publishers Open
Access Journals Please visit our website:
http://lupinepublishers.us/
For more journal
paediatrics and neonatology articles Please Click Here:
https://lupinepublishers.com/pediatrics-neonatal-journal/
To Know More About Open Access
Publishers Please Click on Lupine
Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online


No comments:
Post a Comment