Lupine Publishers | Journal paediatrics and neonatology
Abstract
Case Presentation
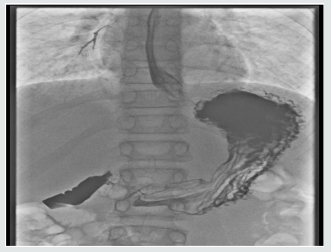
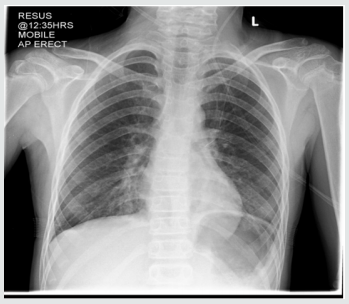
The rest of her systemic review was normal. She was able to eat and drink “normally” but bedside swallow was not formally assessed. She was treated for a respiratory tract infection with intravenous antibiotics and regular salbutamol nebulisers. A few hours later, she developed increased shortness of breath and a peri-arrest call was made. However, examination findings were unchanged, her management remained the same. Her bloods results were Hb 133, WBC 8.9, Plt 293, CRP 5, U&E NAD, LFT NAD. The CXR was reported as left lower lobe atelectasis with an increase of the peribronchial and perivascular interstitial infiltrates (Figure 1). she was reviewed by a second Paediatric Consultant in the ward later, who felt this was more likely to be an upper airway obstruction. He stopped the salbutamol nebulisers, continued the Atrovent nebulisers, started prednisolone and advised to suction intermittently, request an ENT review and arrange a neck X-ray and barium swallow. Neck X-ray was normal (Figure 1). An ENT Consultant reviewed the following day with flexible nasendoscopy which revealed a normal larynx, good vocal cord movement and very slight inflammation on the right arytenoid. The nasendoscopy findings were noted to be insufficient to explain the symptoms. The ENT impression was laryngopharyngeal reflux. She was put on Gaviscon Advance after food and before bedtime. she gradually improved over next three days. She was discharged home on Gaviscon Advance. Barium swallow, done a month later, was reported ‘the mid and distal oesophagus giving a shaggy appearance most likely due to Oesophageal Candidiasis’ (Figure 2).
In view of the barium swallow result she was referred to the Gastroenterologist at the tertiary unit for further investigation and 2 weeks later, underwent an oesophageo-gastro-duodenoscopy, which was normal. The barium swallow images were reviewed by a tertiary radiologist along with the gastroenterologist who raised concerns of aspiration and advised an immediate recall to review the patient. She was reviewed next day, on the pediatric ward. She looked well but continued to complain of ongoing painless dysphagia and muffled voice. A repeat CNS examination revealed bilateral facial weakness, bilateral ptosis with expressionless face, reduced palatal movement and muffled voice (Figures 3 & 4). A clinical diagnosis of Myasthenia gravis was made which was confirmed by EMG next day. Her Acetylcholine receptor antibodies were raised at 3.53 (normal range 0–0.45) confirming the diagnosis of Myasthenia Gravis. Anti-MuSK antibodies were negative. She was commenced on Pyridostigmine 120mg TDS. She was referred to tertiary Neurology unit, where she was admitted 3 weeks later due to deterioration of her symptoms. During this admission oral prednisolone was added to achieve remission. She continued to remain symptomatic, intermittent immunoglobulin infusions were added to her treatment and finally needed partial Thymectomy. She has improved a lot and at present is on Pyridostigmine and reducing regime of oral steroids.
Discussion
Our patient appears to be unique in the literature in her presentation with aspiration pneumonitis. Two cases with foreign body aspiration reported, one in an 8-year-old child2 and the other in a 20-month-old infant [4]. In the former [2] authors emphasize “the importance of considering an undiagnosed neurologic or neuromuscular disease as an underlying cause of foreign body aspiration, particularly if the clinical presentation is in an older child” [2]. This case emphasises the need to think laterally and consider uncommon conditions in the differential diagnosis of a child with a common presenting complaint like acute respiratory distress. This is particularly important if it does not fit with overall clinical scenario. In such cases, We should revisit, take a thorough history and do a full systemic examination including neurological examination.
For more Lupine Publishers Open Access Journals Please visit our website:
http://lupinepublishers.us/
For more journal paediatrics and neonatology articles Please Click Here:
https://lupinepublishers.com/pediatrics-neonatal-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online




No comments:
Post a Comment